Varicocelo or varicocele – what is it?
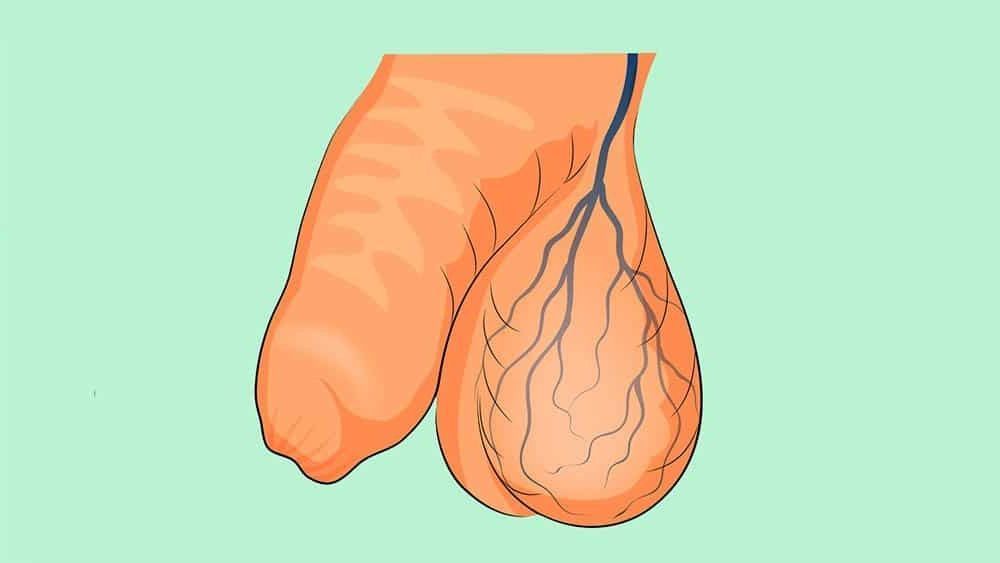
Varicocelum is a clinical entity characterized by a dilation of the veins located at the level of the testicles (veins of the pampiniform plexus of the spermatic cord). These are responsible for draining the blood that vascularizes the testicles. Similar to what happens to the varicose veins of the lower limbs, varicocels consist of “stalwart varicose veins”.
It translates a relatively common congenital anomaly (prevalence documented up to 48% in some series) that arises from valvular incompetence of venous drainage of the spermatic cord. The etiology of varicocels is not fully understood and specific risk factors for their emergence have not yet been identified. Its clinical manifestation usually occurs after 10 years of age – and rarely before adolescence.
In most cases, varicocels are asymptomatic. However, they can be associated with:
· Local symptoms – pain and discomfort, essentially. Pain has a highly variable intensity, tending to worsen when the individual stands or practices physical exercise (as well as throughout the day), and to relieve with the lying position;
· Growth failure and ipsilateral testicular development (testicular atrophy);
· Male subfertility (commitment of sperm production);
· Hypogonadism (commitment to testosterone production).
Varicocels are thought to affect testicular function in a multifactorial way by reducing blood flow to the testicles and by altering the scrotal microenvironment through a thermal increment. Local accumulation of blood in the stolable veins can cause testicular lesions. Consequently, the sperm produced may present changes – quantitative and qualitative – resulting in male subfertility/infertility. Concomitantly, the endocrine function of the testicle (testosterone production) may be equally affected, with hypogonadism. Nevertheless, most young people with varicocels will not have lifelong fertility problems.
Most of them, varicocels are located on the left, given the anatomical characteristics of blood drainage. However, there may be varicocels on the right and bilateral.
The diagnostic evaluation of this clinical entity is fundamentally based on the performance of an objective examination complemented by sonographic evaluation. The objective examination should be performed with the patient standing – a position in which venous dilation becomes more prominent. The testicle on the side of the varicocelum is generally smaller in size.
The imaging evaluation it is necessary whenever the physical examination is not fully enlightening, when the perchronisms admitted in the context of varicocelum remain after surgical correction of the same (to exclude possible recurrence) and in cases of varicocelum on the right which, in extremely rare cases, is associated with the presence of a tumor, which should be excluded.
The classification of varicocelum is relevant in clinical practice:
· Subclinical: non-palpable and non-visible varicocelus at rest or during valsalva maneuver (maneuver to increase intra-abdominal pressure using, for example, a simulation of forced expiration without elimination of expired air), but identifiable in sonographic studies (veins with >a diameter of 3mm);
· Grade 1: palpable varicocelum during valsalva maneuver;
· Grade 2: palpable varicocelum at rest;
· Grade 3: palpable and visible varicocelum at rest.
In most cases, varicocels do not require treatment, justifying only vigilance. However, this may be recommended whenever varicocelum:
· Be painful – and there seems to be no other concomitant pathology that can justify the complaints;
· Condition deficient testicular growth and/or development (testicular atrophy);
· Negatively affect male fertility.
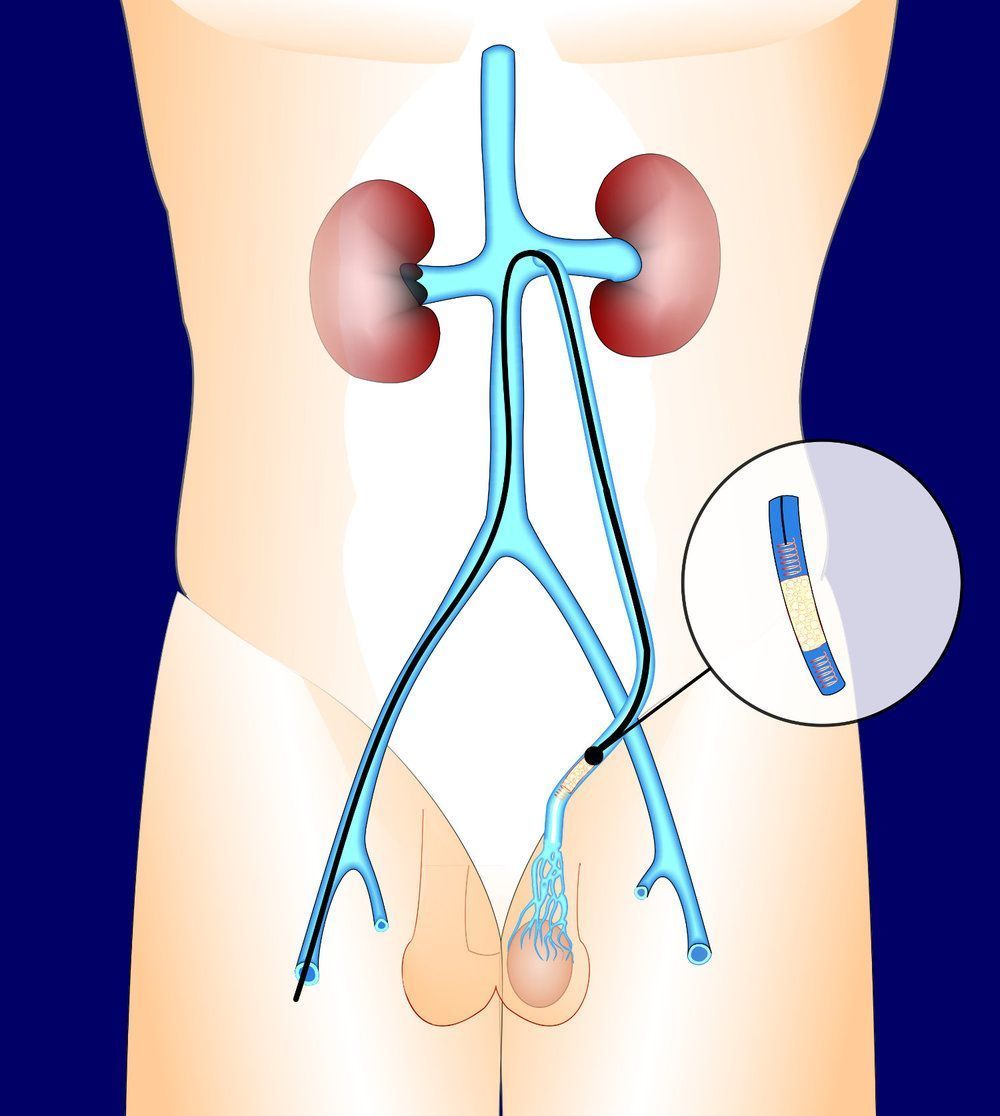
Treatment of varicocelum can be performed by classical open surgery, laparoscopic surgery, microsurgery or percutaneous embolization . The intervention involves “blocking” the veins that drain blood from the testicle and are dilated. This “blockage” redirects blood flow to healthy vessels. The surgical approach can be made from:
· Classical open surgery: a small incision above the groin, more or less at the level of the navel, in the most lateral part of the abdomen;
· Laparoscopic surgery: multiple pericentimetric incisions;
· Microsurgery: a small incision in the groin, in which the procedure is complemented by the use of a microscope.
Alternatively, angiographic occlusion of the varicocelum may be carried out: a substance with specific characteristics is introduced into the dilated vein in order not to block venous flow non-surgically. This technique does not require general anesthesia and is less invasive.
Recovery from surgery is rapid: the patient can resume his normal activity, avoiding significant physical efforts, two days immediately after the intervention, recovering more intense activity about two to four weeks after surgery. The pain resulting from the slight procedure can be stored for weeks to months, and may resolve with general measures such as the use of tight underwear – which allows scrotal elevation – and local application of ice or using analgesics.
The recurrence of the pathology varies between 2 and 20%, depending on the selected technique.