Recurrent, uncomplicated urinary infections in women
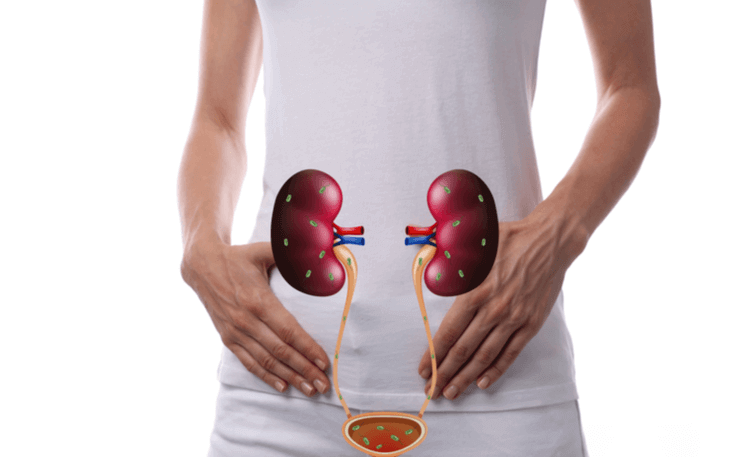
It is known that at least 60% of women will have an episode of urinary tract infection (UTI) throughout their lives, repeating themselves in 20-40%, and up to half of these will have multiple episodes.
They are classified as recurrent ITU’s when there are 2 or more symptomatic episodes in 6 months or at least 3 episodes over a period of one year.
These are very prevalent situations and one of the main reasons for women to resort to medical consultations as they have a significant impact on their quality of life.
The diagnosis of UI refers to a urinary infection in a healthy (non-pregnant) woman with associated symptomatology: ardor urinating, more frequent urination, urinary urgency, presence of blood in the urine and/or onset/worsening of urinary incontinence.
Usually an ITU is diagnosed on the basis of clinical criteria, based on the patient’s symptoms. Uroculture (aseptic urine test) is indispensable in recurrent ITU’s. This analysis identifies the microorganism responsible for the infection and the antibiotics that have the ability to eliminate it, which is essential to adapt the best treatment for each woman. It also allows you to schedule prophylactic treatment or even, in some cases, help in the diagnosis of another underlying condition.
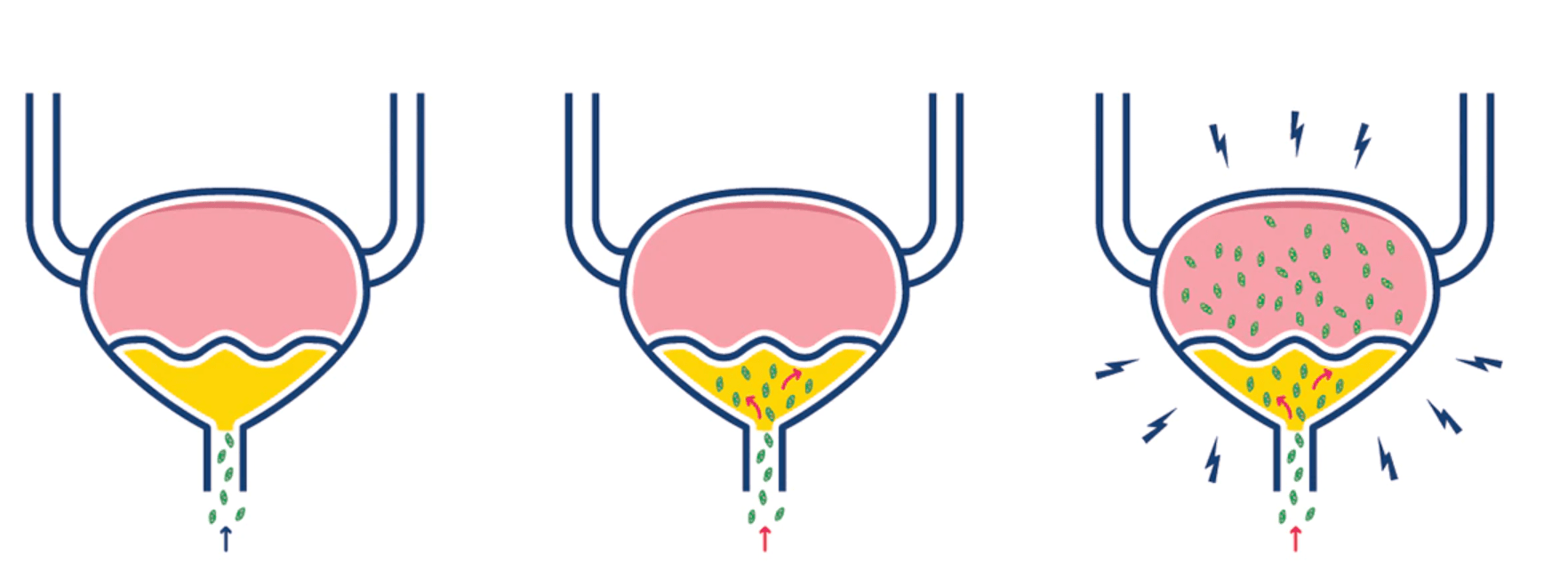
To prevent the emergence of antibiotic resistances it is very important not to treat asymptomatic bacteriurias. This means that healthy women without ITU symptoms do not need to carry out urocultures in regular clinical evaluation. If positive urocultures are identified in asymptomatic healthy women, they have no benefit or require antibiotic therapy.
There are two therapeutic alternatives after uroculture in women with recurrent UIs: either adopt an expectant attitude until the result of uroculture is known or empirical antibiotic is started. The first option is more suitable for women who tolerate symptoms and for whom antibiotic (AB) directed to the identified bacterium is chosen. In the second option, more used in very symptomatic women, an empirical AB is started after urine collection for analysis (without knowing which is most appropriate for that specific bacterium), and then the test result is expected. According to the result of the analysis and clinical evolution of the patient, the physician can later maintain or modify the ab initially proposed.
Resolution of UTI episodes is defined by the absence of urinary symptoms and control urocultures should not be performed after taking AB. As already mentioned, this result may identify asymptomatic bacteriurias that are not indicated for treatment.
Prophylaxis (prevention) of recurrent ITUs has been the subject of study in recent years, with three possible measures to be taken:
- Behavioral changes;
- Non-antibiotic pharmacological prophylaxis;
- Antibiotic prophylaxis.
Behavioral measures include:
- Avoid intimate hygiene products that alter the vaginal flora;
- Adequate hydration;
- Avoid long periods without urinating;
- Urinating after sexual intercourse;
- Avoid vaginal sex after anal sex;
- Avoid the use of spermicides;
- Good hygiene after defecation.
Non-antibiotic pharmacological measures include:
- Pusing: Not all options on the market have clear scientific evidence; have good results and few side effects and do not increase the risk of antibiotic resistance.
- D-mannose: it acts as a defense mechanism against the bacteria’s support to the bladder wall;
- Replacement of vaginal estrogens in postmenopausal women;
Antibiotic prophylaxis includes postcoital antibiotic prophylaxis and continuous daily antibiotic prophylaxis but both should be prescribed in cases exclusively selected by the attending physician.
Dr. Ana Covita
Especialista em Urologia
– Egas Moniz Hospital
– Cuf Cascais
– Cuf St. Dominic of Rana